The NHS Breast Cancer Screening Programme offers screening to all women aged 50-70, every three years. Women aged 71 or over can request screening. Screening saves lives by discovering breast cancer earlier (when it is too small to see or feel), when it is easier to treat.
Easy read guide
Breast cancer
Breast cancer starts when cells in the breast begin to grow in an uncontrolled way and build up to form a lump (also known as a tumour). As the cancer grows, cells can spread to other parts of the body and this can be life-threatening.
Breast cancer is the most common type of cancer in the UK. About 12,000 women in the UK die of breast cancer every year. Survival from the disease has been improving over time, and now about 3 out of 4 women diagnosed with breast cancer are alive 10 years later.
Your risk of getting breast cancer goes up as you get older. About 4 out of 5 breast cancers are found in women over 50 years old. Most women with breast cancer do not have a family history of the disease.
Breast screening
Breast screening uses an X-ray test called a mammogram to check the breast for signs of cancer. It can spot cancers that are too small to see or feel.
Breast screening results
You will receive a letter with your breast screening results within 2 weeks of your appointment. The results will also be sent to your GP.
Occasionally women will need another mammogram before they get their result. Sometimes technical problems mean that the mammogram is not clear enough to read. If this happens, you will be asked to have another mammogram to get a clearer picture of your breast.
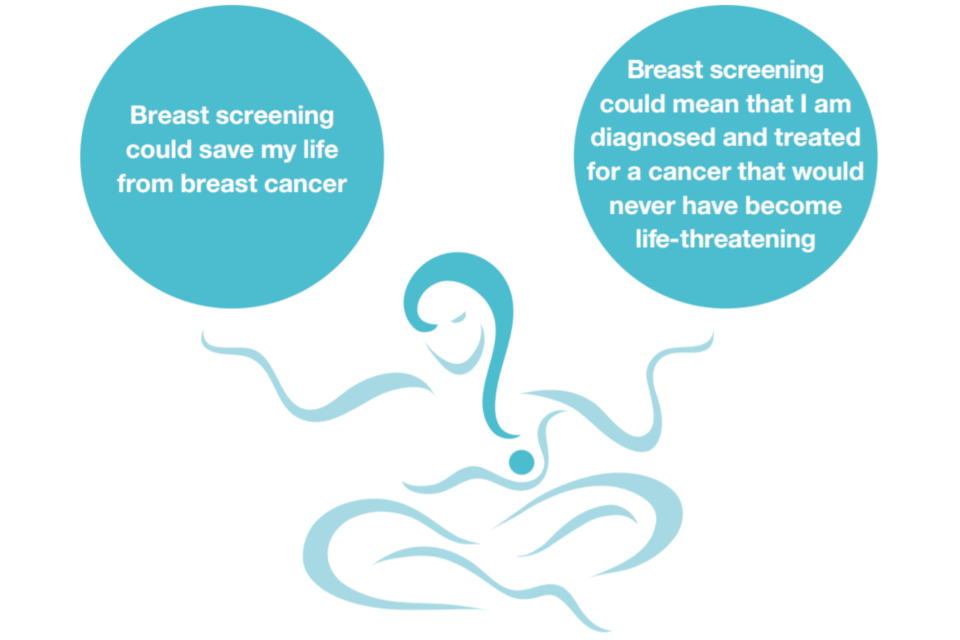
Making a choice: the possible benefits and risks of breast screening
It is your choice whether or not you have breast screening. There are many different reasons why women decide whether or not to have screening. To help you decide, we have included information on the possible benefits and risks.
Screening saves lives from breast cancer.
Lives are saved because cancers are diagnosed and treated earlier than they would have been without screening.
Screening finds breast cancers that would never have caused a woman harm.
Some women will be diagnosed and treated for breast cancer that would never otherwise have been found and would not have become life-threatening. This is the main risk of screening.
Doctors cannot always tell whether a breast cancer that is diagnosed will go on to be life-threatening or not, so they offer treatment to all women with breast cancer. This means that some women will be offered treatment that they do not need.
For more information please visit https://www.nhs.uk/conditions/breast-cancer-screening/. We would encourage you to have screening when you are invited.
Last Update Jan 2022